All published articles of this journal are available on ScienceDirect.
Efficacy and Outcomes of a Novel Telephone-based Gout Disease Management Program
Abstract
Objective:
Gout is the most common inflammatory arthritis in the United States. Despite published guidelines, management remains suboptimal, leading to unnecessary morbidity and increased cost of care. We have designed the gout disease management program (GDMP) to improve outcomes, increase patient satisfaction, and decrease healthcare utilization.
Methods:
Gout patients were seen at their usual rheumatology clinical visit and offered participation in the GDMP. Data were collected between April 2017 and November 2019. Serum uric acid (SUA) levels were measured at the initial outpatient encounter, at the entrance to GDMP, and every 4 weeks until SUA was at the goal of ≤6 mg/dl. Through telephonic encounters, gout-related recent hospitalizations, and ER or urgent care visits since the last encounter were ascertained. Self-reported gout medication usage and adherence were also determined. Patient satisfaction with GDMP was surveyed using a 5-point Likert scale.
Results:
A total of 158 patients were enrolled, of which 112 had ≥ 1 telephone encounter and were included in our analyses. During the telephone phase, 79 patients (70%) achieved the SUA goal of ≤6.0 mg/dl. Only 3 patients (2.6%) required hospitalization or visits to an ER or urgent care center due to gout flare, and 98% rated their encounter as a 5 on the 5-point Likert scale.
Conclusion:
Our telephone-based management program for gout led to improved clinical outcomes as defined by the ACR guidelines, decreased healthcare visits, and had high patient satisfaction.
Significance and Innovations:
• First telephone-based, rheumatology providers-led study to manage gout
• Additional evidence to confirm the feasibility and benefit of telemedicine in common diseases
• First study to show excellent patient satisfaction
1. INTRODUCTION
While gout is an ancient and common inflammatory arthritis, its management remains a clinical challenge [1]. In the United States, controversies regarding treatment strategies are evident in the guidelines of two major institutions [2]. The recently updated American College of Rheumatology guidelines consistently advise a treat-to-target approach, with a goal serum uric acid (SUA) of ≤6 mg/dl [3, 4]. The American College of Physicians recommends basing treatment intensity on minimizing symptoms rather than achieving a SUA goal [5].
Regardless of the guideline applied, evidence indicates that long-term management of gout is infrequently optimized. Treatments that lower SUA are not used regularly, are inconsistently prescribed, and are often under-dosed [6, 7]. Furthermore, patient compliance remains a challenge. First, gout is an episodic disease with long asymptomatic periods between attacks, giving patients the sense that they are well enough which may lead to patients stopping their medication. Additionally, limited access to rheumatology services or time needed away from work in order to travel to a clinic can deter patients from remaining adherent to therapy. Furthermore, lack of patient education regarding gout has been shown to affect compliance [8].
Pharmacist- and nurse-led telemedicine programs aimed at improving gout-related outcomes have been shown to not only improve medication compliance but have also demonstrated effectiveness in increasing the proportion of patients achieving goal SUA level of ≤6 mg/dl [9, 10]. However, to date, healthcare utilization and patient satisfaction with telemedicine programs have not been studied. We designed and instituted a gout disease management program (GDMP) in which the management of gout was initially performed at a standard office visit, and then followed up with a novel telephone-based management program, in which further management with patient education could take place. The objective of the GDMP was to increase the proportion of patients reaching the target SUA goal with resultant clinical control of gout attacks, thus minimizing the need for hospitalization or emergency/urgent care center visits while achieving patient satisfaction.
2. MATERIALS AND METHODS
The GDMP was designed to provide longitudinal care for patients after their usual clinical visits with a rheumatology provider. The treating rheumatologist decided to enroll the patient into GDMP at the initial visit or follow-up visits if the patient agreed to participate in the GDMP. The first patient was enrolled in April 2017, and patients were followed until November 2019. Patients were enrolled regardless of their baseline SUA, and there were no exclusion criteria. This was determined to be an IRB-exempt project (quality improvement project); therefore, written patient consent was not obtained.
2.1. Gout Definition, Telephone Encounters, and Data Collection
The referring rheumatology provider using clinical and laboratory criteria diagnosed gout initially. A crystal-confirmed diagnosis was not made in all cases. The rheumatologist or mid-level rheumatology provider (physician assistant) then followed up with the patient, performing periodic SUA levels and telephone encounters. During the encounters, the following questions were asked: Have you had any recent gout flare or any recent emergency department or urgent care visits due to gout? Have you been taking your gout medications as prescribed? Have you noticed any side effects of your medications? How do you rate your satisfaction with the telephone encounters versus the office visit in managing your gout?
The person who performed the telephone encounters was responsible for modifying treatment, managing side effects, and confirming the adherence to medications. In addition, a visit to the referring rheumatologist was recommended if the telephone encounters were not sufficient to address the clinical issue at hand. The telephone encounters were conducted monthly until SUA level was at the goal of ≤6 mg/dl, and patients were flare free for 3 months (or 6 months for tophaceous gout), then every 6 months for 2 encounters, and finally, yearly if stable.
During the telephone encounters, recent flare and hospitalizations or emergency care visits due to gout since the last encounter were recorded. Additionally, patient’s gout-related medication usage and adherence were monitored by self-report during each phone call. Side effects of medications were documented, and patient satisfaction with the telephone encounters versus usual care office visits was surveyed using a 5-point Likert scale.
A gout flare was treated with either steroids, NSAIDs, or Colchicine. The choice of the medication was left to the discretion of the provider making the phone calls. If the patient develops side effects from the medications used, the referring provider was made aware, and the patient was instructed to follow up with the referring provider.
If a telephone encounter could not be completed easily, a secure email message with the same questions was sent to the patient using electronic health records. If both methods were unsuccessful, an instructional letter was mailed to the patient to contact their rheumatology provider. Patients did not incur any charge for the telephone encounters.
2.2. Urate Lowering Therapy and Prophylactic Medications
Allopurinol was used as the first-line urate-lowering therapy (ULT) of choice. In patients that could not tolerate allopurinol, febuxostat was used instead. Allopurinol’s starting dose was 100 mg daily in patients with an estimated glomerular filtration rate (eGFR) ≥60 ml/min and 50 mg daily in patients with eGFR ≤60 ml/min. If patients were not already taking ULT, it was initiated 2 weeks after an acute flare resolved. Allopurinol doses were increased by 100-mg increments in patients with eGFR ≥60 ml/min and 50-mg increments in patients with eGFR ≤60 mL/min until a goal of SUA ≤6 mg/dl was achieved. In patients receiving febuxostat, the starting dose was 40 mg daily, which could be increased to a maximum of 80 mg daily. Probenecid, at a dose of 500 mg twice daily, was used if both allopurinol and febuxostat were contraindicated.
Colchicine, nonsteroidal anti-inflammatory drugs, or glucocorticoids were used as prophylactic medications to suppress gout attacks with the institution and dose adjustment of ULT. Once target SUA was achieved and maintained for 3 months (or 6 months for tophaceous gout), prophylactic medications were discontinued. Patients were allowed to be on ULT and prophylactic medications prior to entering into the GDMP, but doses were adjusted based on the above as needed.
2.3. Laboratory Monitoring
Complete blood count, creatinine, and liver function tests were obtained at baseline and after 3 months. SUA levels were measured in all patients at their initial outpatient office rheumatology visit, at the time of entry into the telephone phase, and every 4 weeks until SUA was ≤6 mg/dl.
2.4. Patient Education and Medications Refills
Patient education (treat-to-target approach) was provided at the first visit with their office providers and subsequent telephone calls. Medication refills were submitted electronically to the patient’s pharmacy, and SUA laboratory requisitions were sent to the patient by mail or electronically to the lab.
3. RESULTS
As of November 2019, 158 patients were enrolled in the GDMP. A total of 112 patients who had ≥ 1 follow-up in the telephone phase were included here (some patients were not reported here due to the lack of at least one telephone encounter at the time of data extraction). 112 patients were contacted. The mean age at GDMP enrollment was 60 years, and 87% were males. Twenty-six patients (23%) had a crystal-proven diagnosis, while tophaceous gout was diagnosed in 31 patients (27%). A phone call took approximately 5-10 minutes to complete. At least one flare was reported in 25 patients (22%) after entry into the program.
After the initial visit with a rheumatology provider, 108 patients initiated ULT along with appropriate prophylaxis (4 patients either refused ULT or discontinued it without medical input) and reported compliance with the medications. Ninety-one patients (81%) were treated with allopurinol, 16 (14%) with febuxostat, and 1 with probenecid. Colchicine was the most commonly used medication for prophylaxis (n=41, 37%).
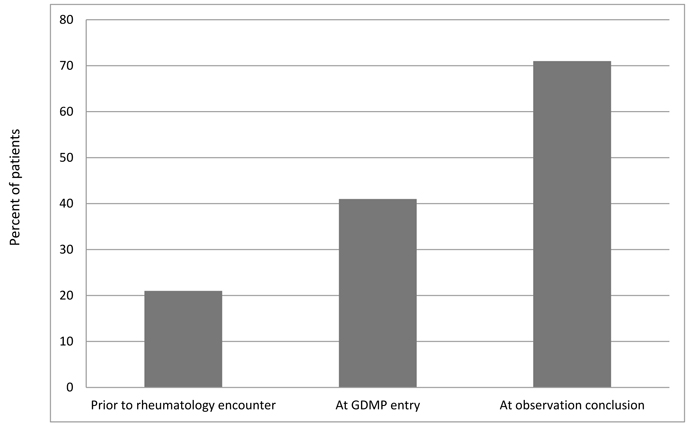
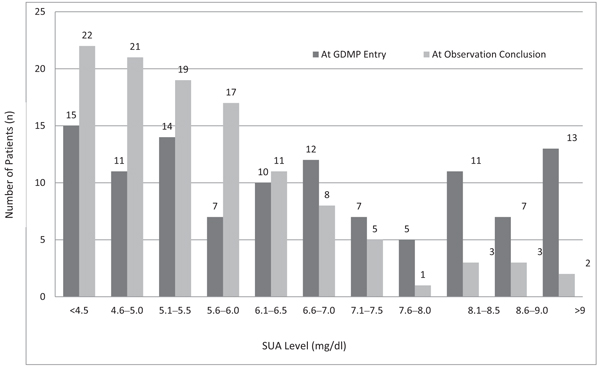
Prior to their first rheumatology visit, 25 patients (22%) had SUA ≤6.0 mg/dl (Fig. 1). At entry in the telephone phase, 47 patients (41%) had SUA of ≤6.0 mg/dl, and by the end of the GDMP observation phase, 79 patients (71%) had achieved SUA goal of ≤6.0 mg/dl. Fig. (2) further delineates and compares the percentage of patients achieving SUA levels, by 0.5 mg/dl intervals, at the start of the GDMP vs. at the end of the study. This figure demonstrates a shift in the distribution to the left, reflecting an increased number of patients with SUA ≤6.0 mg/dl.
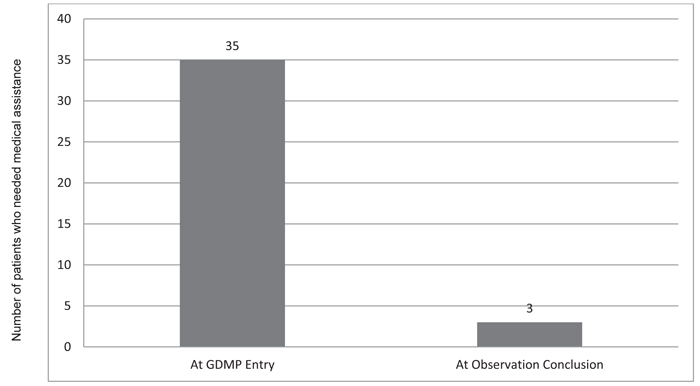
Prior to entry into GDMP, 25 patients (22%) had required emergency or urgent care services due to gout, and 10 patients (9%) had been hospitalized due to gout (Fig. 3). During participation in the GDMP, only 3 patients (2.6%) required an emergency department or urgent care center visit due to gout flare, and none required hospitalization. There were no reported serious side effects from the medications.
Patients were extremely satisfied with the telephone encounters; 98% of patients rated their encounter as a 5 on a 5-point Likert scale.
4. DISCUSSION
We report an effective and well-received follow-up program delivered by telemedicine for medication adjustment and monitoring in the longitudinal management of gout. The goal SUA ≤6 mg/dl was achieved in >70% of patients, and 80% of the patients achieved a more lenient SUA of ≤6.5 mg/dl with good clinical control of their symptoms. Additionally, the majority of patients (86%) were on appropriate prophylactic medications while adjusting the dose of ULT, thereby reducing the likelihood of gout flares. There were no hospitalizations and very few ER or urgent care visits during the observation period of the program. Some patients did not achieve the goal, which is likely due to reasons such as inadequate time in the telephone phase of the study before the study came to a close, inability to reach the patient via phone or other communication methods, and patient noncompliance with medication.
Our program was designed to overcome many obstacles in the longitudinal treatment of gout. Patients were monitored by a series of telephone calls, thus offering convenience to the patient. The provider reinforced medication adherence during the telephone calls, and repeated SUA levels were performed regularly. Patient education was provided, which might have led to better compliance and more frequent achievement of the SUA target. Medication refills were sent electronically with telephone encounters. We used the electronic medical record to contact the patient through messages in cases when phone calls were unavailable as an additional convenience to the patients.
Access to care remains a major issue in rheumatic diseases in the United States due to a nationwide shortage of practitioners. Our GDMP is an ideal way to limit bedside outpatient visit utilization and optimize regular follow-up with a focus on optimizing SUA, targeting a level of ≤6 mg/dl to reduce the likelihood of gouty attacks and long-term consequences of hyperuricemia. Gout is an ideal disease that lends itself to treatment algorithms and telephone-based care with the application of available management recommendations.
The guidelines from the American College of Rheumatology and the American College of Physicians are available for gout treatment [3-5]. Nevertheless, gout treatment remains suboptimal. The reason for this shortfall is likely multifactorial. The lack of symptoms between gout flares decreases patient adherence to chronic daily ULT medications. Additionally, the practitioner’s concern of medication toxicity can lead to using less optimum doses of medication. Furthermore, the frequent need to adjust the dose of medications and obtain SUA level (which typically requires multiple office visits) is an obstacle to many patients due to time constraints. Lastly, the treat-to-target approach, which is adopted by most rheumatologists as advocated by the ACR guidelines [3, 4] is not necessarily embraced by primary care providers based on the prior 2017 ACP guidelines [5].
Similar to our study, in the RamP-UP study, patients were contacted directly by pharmacists [9]. The SUA goal of ≤6 mg/dl was achieved in 30% of patients in the intervention group, in comparison to only 15% in the usual care group. Adherence was also higher in the intervention group. The intervention period was one year only. Our results differed from the RAmP-UP study. We did not use an automatic voice response system; rather, we called the patients individually, which might have led to a more aggressive lowering of the SUA in our trial. Furthermore, our observation period was longer, and a rheumatology provider performed the intervention.
In a study by Doherty et al. [10], a nurse-led intervention was successful in obtaining a goal SUA ≤6 mg/dl in 95% of the patients after 2 years. Of note, in that study, telephone contact could be substituted for face-to-face visits, and home visits were permitted. In our study, patients were mostly newly diagnosed, which require frequent adjustments in medication doses and frequent encounters, while in the study by Doherty et al., patients were mainly established patients with a mean duration of disease of 11 years. Furthermore, the higher percentage of patients achieving target SUA in the Doherty et al. study as compared to ours could be related to our rheumatology providers doing the intervention as part of their clinic duty to mimic real-life situations, while the study by Doherty et al. had an educated nursing staff dedicated to this study. Additionally, after entry into the telephone phase of the program, we did not conduct any face-to-face or home visits as in the study by Doherty et al., which could also have led to a higher percentage of patients achieving target SUA in their study versus ours.
A study by Yokose et al. [11], in which an e-visit conducted in 62 patients with gout was compared to a matched historical cohort, showed that SUA target of ≤6 mg/dl was obtained in 63% of patients in the intervention group versus 33% in the historic matched group. Our results were superior, likely because the Yokose et al. study used email reminders and questionnaires while we conducted phone calls in real-time with patients.
There are several strengths to our study. Patients were enrolled after a visit with their rheumatology provider, which makes gout less likely to be misdiagnosed. We used real-time phone calls instead of automated contacts with patients, which might have increased the rate of patient compliance. After usual face-to-face office visits, the patients were entered into a novel telephone phase of the program. This was very convenient for patients, which in turn led to higher patient satisfaction. We were able to achieve a goal SUA level ≤6 mg/dl in the majority of patients, and the rate of hospitalizations, ER, or urgent care visits due to gout was very low. We included a large number of patients in our study, and providers continued to refer patients to our study. This study was the first of its kind to employ telephone-based, guidelines-directed management prospectively led by rheumatology providers.
One limitation of this study was reaching patients by phone. There were incidences where patients were not available by phone, and we were forced to use our electronic medical record and mailing system trying to contact such patients. Additionally, repeated SUA levels were not always done on time after adjusting the medication dosage due to patient factors. Furthermore, we did not have a control group in our study, and as such, we cannot draw definitive conclusions about the efficacy of this program compared to the standard of care. Furthermore, we performed the telephone encounters free of charge, but this may not be plausible at all institutions. There is also a possibility of enrollment bias as our patients were included based on the discretion of the initial rheumatology provider. Finally, there was no time-related data at the entry on prior healthcare utilization.
CONCLUSION
Our study demonstrated that a gout disease management program consisting of typical visits with a rheumatologist followed by a novel telephone-based follow-up phase has a high patient satisfaction rate. It may lead to improvement in following clinical guidelines, thus leading to better management of disease and reduced healthcare costs. Such visits can reduce outpatient office visits, with a more abbreviated management strategy by phone, thus freeing time to provide access to patients requiring bedside encounters. While providers were not reimbursed for doing such calls, new COVID-19 related changes in reimbursement for telemedicine care may change this in the future. Future work with a comparable group that can assess the effect on healthcare expenditure is warranted to further elucidate the benefits of a GDMP for gout management.
AUTHORS' CONTRIBUTIONS
AA contributed to the acquisition, analysis, interpretation of data, of data, drafting and substantial revision of the work. AA approved the submitted version.
GL contributed to the acquisition and analysis of the data. GL approved the submitted version.
WTA contributed to the design, acquisition, analysis, interpretation of data, and substantial revision of the draft. WTA approved the submitted version.
ETHICAL STATEMENT
This was determined to be an IRB-exempt project; therefore written patient consent was not obtained. This was determined to be a quality improvement project.
CONSENT FOR PUBLICATION
Not applicable.
AVAILABILITY OF DATA AND MATERIALS
The data sets analyzed during the current study are available from the corresponding author [A.A.H] on reasonable request.
FUNDING
None.
CONFLICT OF INTERESTS
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


