All published articles of this journal are available on ScienceDirect.
The Protein Tyrosine Phosphatase Non-receptor Type N22 (PTPN22) Gene Functional Polymorphism (1858T) is not Associated with Rheumatoid Arthritis in Kuwaiti Patients
Abstract
Background:
Rheumatoid Arthritis (RA) is a chronic disorder characterized by an inflammation of synovial tissue in joints resulting in pain, deformities and affects the quality of life. The gene for protein tyrosine phosphatase non-receptor type 22 (PTPN22) encodes a lymphoid specific phosphatase (LYP), which serves as a negative regulator of T lymphocyte activation and is associated with a number of autoimmune/chronic diseases in various ethnic groups.
Objective:
This study was undertaken to investigate an association between PTPN22 gene functional polymorphism (C1858T; rs2476601) and rheumatoid arthritis (RA) in Kuwaiti Arabs. The frequency of this candidate locus was compared between Kuwaiti RA patients and the controls and with that reported from other populations.
Methods:
The study was carried out in 191 Kuwaiti RA patients and 214 healthy controls. The diagnosis of RA was carried out according to the guidelines of the American College of Rheumatology (ACR). The genotypes of PTPN22 gene (C1858T) polymorphism were detected by polymerase chain reaction-restriction fragment length polymorphism (PCR-RFLP) and confirmed by DNA sequence analysis in RA patients and controls.
Results:
The TT genotype of PTPN22 gene functional polymorphism C1858T was found in 2/191 (1%) in RA patients compared to 2/214 (1%) in the controls (P = 1.0). In contrast, heterozygous CT genotype was detected in 3/191 (1.57%) RA patients compared to 32/214 (14.9%) in the controls. The CC genotype was detected in 186/191 (97.38%), RA patients while it was detected in 180/214 (84.1%) of the controls. The two RA patients who carried the homozygous variant (TT) genotype were both positive for rheumatoid factor (RF) and did not have any extra-articular manifestations. Amongst the Kuwaiti RA patients, 27% had a family history of RA. No correlation was found between the activity/severity of the disease and PTPN22 gene polymorphism genotypes.
Conclusion:
This study did not find an association between the PTPN22 gene functional polymorphism (C1858T) and clinical manifestation and activity/severity of RA in Kuwaiti Arabs. This is in sharp contrast to previous reports from Caucasian and some other populations in which a positive association of PTPN22 gene (C1858T) polymorphism with genetic susceptibility to RA has been reported.
1. INTRODUCTION
Rheumatoid Arthritis (RA) is a systemic, autoimmune, chronic disorder that results in joint inflammation and the surrounding tissues. The disease symptoms include tenderness, stiffness, swelling, pain, and finally, the loss of function of joints [1]. It has been suggested that RA is a complex disease that is caused by an interaction between a number of genetic loci and environmental factors [2]. It has been reported in previous studies that genetic factors contribute to approximately 50-65% of the risk of having RA [3, 4]. A functional polymorphism (C1858T resulting in R620W) in the protein tyrosine phosphatase non-receptor type N22 (PTPN22) gene (rs2476601) has been shown to be associated with a number of chronic diseases with auto-immune involvement [5, 6]. PTPN22 gene is located on chromosome 1p13.3-p13.1 and encodes a lymphoid-specific phosphatase (Lyp). The Lyp serves as a negative regulator of T-cell activation and differentiation [7]. It has been shown that PTPN22 modulates T cell receptor (TCR) signaling pathway by regulating the phosphorylation of its downstream substrates such as Lck, Zap70, Vav etc [8]. The Trp (T-) allele has been shown to be associated with impaired binding between Lyp and the SH3 (Src homology 3 domain) of CsK, which is a crucial suppressor of kinases that mediate T cell activation [8]. Previous studies on the association of PTPN22 gene (C1858T) polymorphism and RA in different ethnic groups/populations have yielded contradictory findings [9]. Fodil et al. [10] have reported a significant and strong association between PTPN22 gene (C1858T) polymorphism and RA in the Western Algerian population. In contrast, this polymorphism was detected in only two RA patients from Egypt (only in heterozygous state) and in none of the controls [11]. However, another study from Egypt, reported an association between PTPN22 gene +1858T allele and RA patients from Nile delta [12]. A study from Iran did not find an association between the PTPN22 gene polymorphism and RA and detected only homozygous CC genotype in all patients and controls; the genotypes with variant allele (TT or CT) were not detected at all [13]. A significant association between PTPN22 gene polymorphism and RA was reported in a population from UK [14]. Positive association between PTPN22 gene C1858T polymorphism and four autoimmune diseases, RA [15], SLE [16], autoimmune thyroid disease [17] and type 1 diabetes mellitus has also been reported [18-20]. In a study from Western Mexico, an association between PTPN22 gene polymorphism and the onset of RA has been reported but not with clinical activity or functional disability resulting from RA [21]. No association between any of the PTPN22 gene polymorphisms and RA was reported in Blacks from South Africa [22]. These conflicting findings have been considered to be due to various causes such as clinical or genetic heterogeneity, small sample sizes, racial or ethnic differences [23]. Therefore, it is important to assess ethnic-specific associations to evaluate the nature of genetic associations in different populations. In this study, we have investigated whether the PTPN22 gene (1858T) functional polymorphism contributes to genetic susceptibility of RA in a completely different population (Kuwaiti Arabs).
2. MATERIALS AND METHODS
The study included 191 Kuwaiti RA patients who attended the Rheumatic Disease Unit of Amiri Teaching Hospital, Kuwait over a period of one year. All patients fulfilled the American College of Rheumatology (ACR) classification criteria for RA [24] and gave informed consent for participation in the study. A complete clinical assessment was done for the RA patients. Standardized joint counts and patient’s ratings of general health on a 100 mm visual analog scale were recorded. The data was collected and stored in a predesigned form. The four-variable Disease Activity Score 28 (DAS28-CRP) was computed using the formula described earlier [25]. To define remission, a cutoff point of <2.6 was used for the DAS28-CRP, and it corresponded with modified American Rheumatism Association criteria for the remission [26, 27]. The patients were characterized on the basis of disease duration into having early (<3 months), established (>3 months to up to 2 years), or late (>2 years) disease [28, 29]. These clinical subdivision of RA patients corresponded with the maximum number of joints involved at any stage into mild (3-6 joints), moderate (>6 but <20 joints) or severe (>20 joints) disease, respectively [29-31]. Radiological investigations of hands, writs and feet were performed and read by a blinded radiologist to assess RA erosions. The strategy for the treatment of RA patients was based on the published guidelines [32]. The RA patients received treatment with Disease Modifying Anti-Rheumatic Drugs (DMARD) and/or biological, and when appropriate, Non-Steroidal Anti-Inflammatory Drugs (NSAID) and/or corticosteroids were also used. Healthy volunteers (Kuwaiti Nationals) matched for age, gender and ethnicity were used as controls in this study. The control subjects were examined by a trained Rheumatologist to ascertain their health status.
2.1. Genotyping
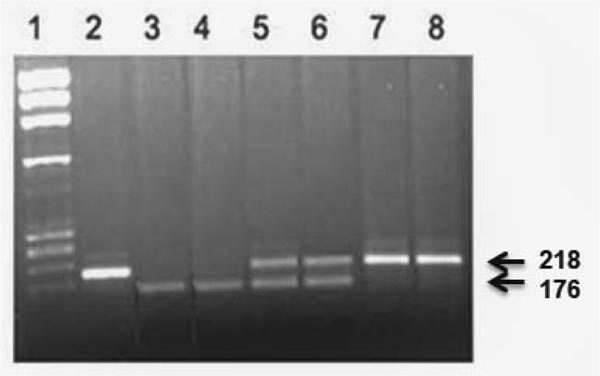
Venous blood (approximately 5 ml) was collected from RA patients and controls in EDTA tubes. The genomic DNA was isolated by an already published method [33]. The genotypes of (C1858T, rs2476601) functional polymorphism of the PTPN22 gene were detected by polymerase chain reaction-restriction enzyme fragment length polymorphism (PCR-RFLP) method as described earlier [34]. A 218 bp DNA fragment was amplified by using the primers: Forward primer: 5’- ACTGATAATGTTGCTTCAACGG-3’ and reverse primer: 5’-TCACCAGCTTCCTCAACCAC-3’. The PCR mixture contained 10x PCR buffer (Applied BioSystems, Foster City, USA); 1.5 mM MgCl2; 0.2 mM of each of the dNTPs (deoxyribonucleotide triphosphates); 20 pmol of each primer, 250 ng template DNA and 1U Taq DNA polymerase (VWR Life Sciences). The amplification conditions used were the same as described earlier [34]. The products of PCR amplification were cleaved with restriction enzyme RsaI at 370C for 90 min. The digestion products were separated by 2% agarose gel electrophoresis. The staining was carried out with ethidium bromide and visualization was done under the UV light. An example of detection of PTPN22 genotypes by PCR-RFLP analysis is presented in Fig. (1). In individuals who carried the T-allele, the RsaI restriction enzyme site was absent from 218 bp PCR product, while in individuals with C-allele, two cleavage products of 176 bp and 42 bp were detected. The heterozygous individuals carried all three cleavage products (218 bp, 176 bp and 42 bp). The genotypes were confirmed by determining the sequence of PCR products using an ABI 3130 genetic analyzer.
2.2. Statistical Analysis
Statistical Package for Social Sciences version 23 (SPSS, Chicago IL, USA) was used to analyze the data. The genotype and allele frequencies from RA patients and controls were calculated by direct counting. The confidence interval (CI) was set at 95% and statistical significance was set at P <0.05 (two-tailed). In order to determine the statistical significance of differences in genotype/allele frequencies between RA patients and controls, the Fisher’s Exact test was used. The statistical significance was determined using two models (the ‘co-dominant’ and the ‘dominant’ model). The genotype frequency in homozygous CC subjects and the ‘C’ allele frequency were considered as reference (assumed to be associated with the least risk of RA) for calculation of the statistical significance in co-dominant and dominant genetic models. In the dominant model, the genotype frequencies of CT and TT were pooled (RA patients having at least one variant allele of the PTPN22 gene rs2476601 polymorphism).
3. RESULTS
The RA patients group (total 191) consisted of 164 females and 27 males, with a female to male ratio of 7:1. The mean age of Kuwaiti RA patients was 54.65 years ± 13.16 and mean duration of disease was 9 years (± 7). In 149/167 (89%) RA patients, the disease was classified as seropositive, while 18 RA patients (11%) were seronegative (some clinical data was not available from 24 RA patients). The evaluation of joints by radiography revealed erosive disease in 31/167 (19%) RA patients whereas 136 (81%) patients had no evidence of bone erosions. Only 8/149 (5%) RA patients had extra-articular manifestations and in 141 patients (95%) the RA was limited to the joints. In patients who manifested extra-articular manifestations, 6/8 had Sicca/Sjogren syndrome and one had autoimmune uveitis. The family history of the disease was noted in 52/191 (27.23%) RA patients who had one or more immediate members of their family affected with RA.
The three PTPN22 genotypes i.e. TT, CT and CC were identified on the basis of characteristic pattern of bands in RA patients and the controls by using PCR-RFLP method as described in Materials and Methods section. The homozygous variant TT genotype of PTPN22 gene polymorphism was detected in 2/191 (1%) Kuwaiti RA patients compared to 2/214 (1%) in the controls (Table 1). In contrast, the heterozygous CT genotype was detected in 3/193 (1.57%) RA patients compared to 32/214 (14.9%) in the controls (Table 1). The CC genotype was detected in 186/191 (97.38%) of the RA patients while it was present in 180/214 (84.1%) of the controls. Two RA patients who carried the homozygous variant ‘TT- genotype’ were both positive for rheumatoid factor (RF) and did not have any extra-articular manifestations. The frequency of C-and T-alleles of the PTPN22 gene (C1858T) polymorphism amongst Kuwaiti RA patients and controls is also presented in Table 1 (lower part). Although the difference between the variant T-allele was statistically significant between RA patients and controls, the frequency was considerably higher in the controls (Table 1). No correlation was found between the PTPN22 gene polymorphism genotypes/alleles and the activity or severity of the disease in Kuwaiti RA patients. The majority (186/191) of the RA patients had a CC genotype irrespective of the RA activity and/or severity.
|
Genotype/ Alleles |
RA Patients N=191 (%) |
Controls N= 214 (%) |
OR (95% CI)* | P-value** |
|---|---|---|---|---|
| Co-dominant | ||||
| CC | 186 (97.4) | 180 (84) | 1.00 (Reference)a | |
| CT | 3 (1.6) | 32 (15) | 0.09 (0.027 – 0.301) | <0.0001** |
| TT | 2 (1.0) | 2 (1.0) | 0.97 (0.134 – 6.947) | 1.00 |
| Dominant | ||||
| CC | 186 (97.4) | 180 (84) | 1.00 (Reference)a | |
| CT/TT | 5 (2.6) | 34 (16) | 0.14 (0.154 – 0.372) | <0.0001** |
| Alleles | N = 382 (%) | N = 428 (%) | ||
| C | 375 (98.2) | 392 (91.6) | 1.00 (Reference)a | |
| T | 7 (1.8) | 36 (8.4) | 0.20 (0.089 – 0.462) | <0.0001** |
4. DISCUSSION
The results presented in this study are in sharp contrast to those reported in previous studies from European and some other populations where an association of RA with T allele/TT genotype of the PTPN22 gene has been reported [12]. The C1858T, resulting in R620W; rs2476601 is a functional polymorphism in the PTPN22 gene and is considered as a significant common risk factor in other auto-immune diseases besides RA, these include, Juvenile idiopathic arthritis, Systemic lupus erythematosus (SLE), Graves’ disease, Systemic sclerosis, Generalized Vitiligo, Type-1 diabetes mellitus, Hashimoto thyroiditis, Addison’s disease and Myasthenia gravis [15-20]. A meta-analysis of the RA genome-wide-association studies (GWAS) demonstrated that R620W variant of the PTPN22 gene was indeed associated with susceptibility to RA [35]. Although T-allele of the (C1858T) polymorphism in PTPN22 gene was identified as a risk allele in the above studies, a wide variation in T-allele frequency was reported in different populations [14]. The frequency of T allele was found to be 12% in North Europe, while in South Europe, it was reported to be 6% [36]. Several previous studies have reported a significant positive association between PTPN22 gene (C1858T) polymorphism and RA from a number of European and other populations, which include French [37], UK [15], Finnish [38], Swedish [39], German [40], Dutch [41], Spanish [42] and Canadian [43] populations. A study from Mexico reported a strong association between T-allele of the PTPN22 gene (C1858T) polymorphism and RA and claimed that this behaves like a dominant variant, conferring increased risk of the disease [22]. However, the same study reported no significant association of RA with homozygous TT genotype of the PTPN22 gene polymorphism, which the authors attributed to low frequency of this genotype in the Mexican population [22]. Similar findings showing positive association of T-allele with RA have been reported in patients from Columbia [44]. Although a positive association between PTPN22 gene (C1858T) polymorphism with RA has been reported from Algeria [10], two other studies from nearby Tunis have reported contradictory findings. While “no association was reported by Sfar et al. [45]”, Chabchoub et al. [46] reported a positive association between PTPN22 gene (C1858T) polymorphism and RA in similar case-control studies from Tunisian population. In contrast, this polymorphism was found to be extremely rare in East Asian and African-American populations [47-50]. Nabi et al. [9] reported results of their meta-analysis, which revealed that the PTPN22 1858T allele was not associated with an increased or a decreased risk of RA in Asian populations. Whereas in the same study [9], when the results were stratified by ethnicity, a statistically significant relationship between the PTPN22, TT genotype and RA risk was detected in the Caucasian populations. On the basis of this meta-analysis, the authors postulated that the prevalence of C1858T polymorphism in the PTPN22 gene in a general population/ethnic group could be the determinant of its correlation with the RA [8]. This inference is also supported by the data from PTPN22 gene association studies with RA in Mexicans where although significant difference between the variant T-allele was detected between RA patients and controls, there was no significant difference between genotypes which the authors suggested to be due to low prevalence in their population [22]. Our data from Kuwaiti RA patients, like the report from Mexico [22] also revealed a rather low prevalence of the T-allele in RA patient cohort compared to the controls. However, the data from Kuwait differed from that reported from Iran [13] in which the T-allele was not detected at all.
The effect of T-allele of the PTPN22 gene on RA severity, its activity and disease progression is not clear [9]. In an earlier study, no association between the T-allele and the rate of joint destruction was detected [51]. However, another study revealed an association between the presence of the PTPN22 T-allele and a higher rate of structural damage [52]. Our results from RA patients like those reported from Mexico [22] did not find any correlation between the T-allele and either activity or severity of the disease in Kuwaiti Arabs.
CONCLUSION
The findings reported in this study showed the lack of association between PTPN22 gene (C1858T) functional polymorphism and genetic susceptibility to RA in Kuwaiti Arabs, unlike the Caucasians and some other populations in which an association has been reported. No correlation was detected between the PTPN22 gene polymorphism genotypes and the activity or severity of the disease in Kuwaiti RA patients.
AUTHORS' CONTRIBUTIONS
Conceptualization: MZH, AMA
Data curation: MZH
Formal analysis: MZH, AMA
Funding acquisition: Not applicable
Investigation: AMA, MZH, JS, EAHH, YAB
Methodology: AMA, MZH, JS, EAHH, YAB
Statistical analysis: JS, MZH
Resources: AMA, MZH, EAHH, YAB
Supervision: MZH
Writing – original draft: MZH
Writing – review and editing: MZH, AMA. All authors read and approved the manuscript.
LIST OF ABBREVIATIONS
| RA | = Rheumatoid Arthritis |
| PTPN22 | = Protein Tyrosine Phosphatase Receptor Type N22; |
| PCR | = Polymerase Chain Reaction; RFLP, restriction fragment length polymorphism; |
| RFLP | = Restriction Fragment Length Polymorphism |
| RF | = Rheumatoid Factor |
| ACPA | = Anti-Citrullinated Protein Peptide Antibody |
| ACR | = American College of Rheumatology |
| GWAS | = Genome Wide Association Study |
| SNP | = Single Nucleotide Polymorphism |
| UV | = Ultra-Violet |
| bp | = base pair |
| CI | = Confidence Interval |
| OR | = Odds Ratio |
| STAT4 | = Signal Transduction and Activation of Transcription-4 |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The Ethics Committee of Health Sciences Centre, Kuwait University, approved this study (Ref. No. VDR/MED/38576).
HUMAN AND ANIMAL RIGHTS
No Animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Written informed consent was obtained from all the study subjects included in this study.
AVAILABILITY OF DATA AND MATERIALS
The corresponding author [M.Z.H] would make the data available upon request.
FUNDING
The study is funded by Kuwait University, General budget (# Med.2019).
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
We would like to thank the study subjects (RA patients and controls) for participation and hospital staff for their assistance in this study. The help from Mrs. Asiya T. Mohammed in the statistical analysis of data is thankfully acknowledged.


