All published articles of this journal are available on ScienceDirect.
Direct Costs of Rheumatoid Arthritis among Patients with Biological Therapy in Morocco: ECORAM Study
Abstract
Objective
The present study aims to estimate the annual direct costs of rheumatoid arthritis (RA) among patients with biological therapy in Morocco from the societal perspective and, to identify factors affecting the increase of direct costs.
Methods
This is a descriptive, observational, and ambispective cohort study which was accomplished over one year, from July 2019 to October 2020, with a follow-up after 6 months since the inclusion’s date. study, conducted in 110 patients with RA and under BDMARDs from July 2019 until October 2020. The data collection was done by face-to-face interviews using a questionnaire. Additional information was obtained from the patient’s files.
Results
The mean age of patients was 50.5 years old with 85% of women. The annual average total direct costs are $7,659 with a minimum and a maximum of $1,889.5 and $29,158.3 respectively. The medical costs represent 98% with the majority of BDMARDs (67%) at $4,944.73, followed by hospitalization costs (12%) at $889. The remaining 20% includes the other costs ($1,825). The RAMED (Régime assistance Médicale) paid around 47% of the total medical costs which is $3,445.56, and the health insurance organizations (CNOPS, CNSS, private insurance) paid $2,876.7 (39%), while patients paid $1,048.65 (14%) on medical and non-medical costs. The following factors were significantly associated with total direct costs of RA: marital status, number of children, working status, monthly household income, medical insurance, disease duration, to undergo surgery, DMARDs, NSAIDs and antalgic, and the class of BDMARDs.
Conclusion
The economic burden of RA is very high for the study population since the majority are vulnerable and have a monthly household income of less than $250. Further, two-thirds of patients had the RAMED, which supports almost all the medical costs. However, the costs paid by the patient are about one third of their annual household income.
1. INTRODUCTION
Rheumatoid arthritis (RA) is the most frequent form of chronic inflammatory arthritis. It is an autoimmune progressive disease, characterized mainly by inflammation, joint destruction, and pain. These features cause a functional disability and impact negatively the patient´s and the family´s quality of life [1]. The prevalence of RA in most world regions is under 1% of the population [2] with an incidence of 0.2% to 0.5% [1]. According to a recent study, the worldwide prevalence was 460 per 100,000 population between 1980 and 2018, with a confidence interval of 95% (0.06-1.27) [3].
The progression of RA takes several years, gradually affecting different sets of joints. There is currently no recognized etiology for RA. Genetic (hereditary) predisposition, and infections from measles, and mumps, may be some of the factors that contribute to the onset of the condition [4]. Children and the elderly are not immune to the disease, which can strike at any age. Although it is most common between the ages of 40 and 60. The frequency of RA is greater in women than in males, rises with age, and varies by race [5].
The symptoms of RA might vary. It can be manifested by joint pain and stiffness in the morning for more than thirty minutes. as well as joint discomfort and trouble moving in it. Malaise, weight loss, and overall weakness may also accompany RA, particularly during exacerbations. RA patients may have fluctuating levels of inflammation, with periods of improvement depending on the disease stage. One-fifth of persons with RA develop rheumatoid nodules, which are rather thick structures under the skin, frequently around joints or in regions of pressure and friction [4].
Even with the important improvements in medicine today, RA remains an incurable disease. The introduction of innovative therapies has significantly improved the clinical expectations of patients and physicians. However, the extremely high cost of these biological agents, the side effects monitoring, and the frequent visits required for rigorous disease control result in a significant increase in healthcare utilization and costs high for all the stakeholders; RA patients, the ministry of Health, and health insurance organizations [6].
In Morocco, the incidence of the disease is not established. The first publication on RA dates from the 1960s [7]. Subsequent studies have reported data on the frequency and specificities of the disease. They showed that chronic inflammatory rheumatism accounted for about 21.5% of rheumatic pathologies seen in rheumatology, with RA alone accounting for 38.5% of cases. They also show that RA in Morocco started earlier and had fewer extra-articular manifestations than the forms described in Europe [8-10]. More recently, interest in the disease has grown with the development of rheumatology and other studies have focused on various aspects of the disease, including its socioeconomic impact [11, 12].
The Moroccan model of basic medical coverage (BMC) adopted during the study period is based on a mixed system composed of two poles: CHI (Compulsory Health Insurance), and RAMED (Medical Assistance Program) [13, 14]. The BMC gathers the insured persons of the CNSS (National Social Security Fund) and those of the CNOPS (National Fund of Social Security Organizations), in addition to private insurance [15, 16]. The reimbursement rate of the CNSS for RA classified as a long-term disease is capped at 93% of the NRP (National Reference Pricing) (CNSS official website). The reimbursement rate of the CNOPS for RA as a long-term disease, is capped at 100% of the NRP. (CNOPS official website). In the case of private insurance, the rate of reimbursement depends on many factors; the contribution rate of the member, the contribution rate of the, recruiter and the insurer company type, It can be up to 100%. As regards the RAMED, established in 2011, offers an undeniable advantage to a large population of the poor and vulnerable. The beneficiary has free access to all public healthcare services: (Consultations, Hospitalizations, biological and radiological assessments, as well as BDMARDs available at the hospital pharmacy). However, no refund will be available for all medicines purchased from private pharmacies or medical services performed in the private sector [17]. In Morocco, a study conducted in 2020 was the first to provide the annual direct costs of biological therapies related to RA. However, the study was retrospective and data was not exhaustive since it was collected from the Moroccan registry of biological therapies in rheumatic diseases (RBSMR Registry) [11].
Therefore, the main objective is to estimate the annual direct costs related to RA among patients treated with biological therapy in Morocco from a societal perspective, while also identifying factors affecting the increase of direct costs. To our knowledge, this study is the first in Morocco to report all medical direct costs collected exhaustively from both patients and related files.
2. METHODS
2.1. Study Design and Population
ECORAM is a descriptive, observational, and ambispective cohort study conducted at the rheumatology departments of ELAYACHI Hospital during consultation or hospitalization. One hundred and ten patients with rheumatoid arthritis were recruited randomly and agreed to participate in this study, which was accomplished over one year, from July 2019 to October 2020, with a follow-up after 6 months after the inclusion date.
All patients had been diagnosed by a rheumatologist based on clinical, biological, and imaging data. Their diagnoses also fulfill the American College of Rheumatology (ACR) criteria [18]. Patients older than 18 years with a confirmed diagnosis of RA treated with one of the BDMARDs available in the hospital’s pharmacy and followed in one of the rheumatology departments of EL AYACHI hospital, were included in this study. The Patients who were prescribed biotherapy for any other indication than rheumatoid arthritis or who were less than 18 years old were excluded.
2.2. Data Collection
An assessment questionnaire was developed and tested on a sample of patients to assess a patient’s comprehension and adjusted before the launch of patient recruitment. We collected relevant information for the study from the case files and available medical records from hospital registers or the hospital informatic system (HIS). Characteristics such as age, sex, weight, height, educational level, work status, marital status, kind of health insurance, monthly income, duration of illness, and other data related to medical and non-medical costs were collected through a questionnaire during a face-to-face interview with the patient, assisted by the same investigator for all recruited patients
All medications purchased from the pharmacy were reported by the patient himself, and confirmed by the medical prescription on the patient’s file. The prices were collected from the national site “www.médicament.ma”. The BDMARD’s prices correspond to the real purchase price communicated by the hospital pharmacy during the study period.
2.3. Direct Cost Categories and Estimation
The direct medical costs were calculated by applying the sum of the different healthcare services used in the context of RA, whether in the public or private sector during the year of the study. Hence, we distinguished 10 categories: physician visits, hospitalizations, Radiology, laboratory analysis, conventional treatment “DMARDs”, biological agents “BDMARDs”, medications (non-steroidal anti-inflammatory drugs NSAIDs), analgesics drugs, surgery, medical equipment, and physiotherapy.
The cost of transportation for travel to the health centers was considered a direct non-medical cost. The costs considered in the public sector are those defined by the National Reference Rates for each procedure and each patient’s affiliation. The costs considered in the private sector are those communicated by the patients.
The costs considered in this study were collected over a one-year period. Two interviews were held with each patient, at inclusion, costs for the last 6 months were collected, and then a follow-up interview was held to collect data on expenses for the following 6 months.
All The costs were presented in American dollars (USD) according to the exchange rate in 2023 (1 Moroccan Dirham=$0.0985, without inflation adjustment).
2.4. Ethical Approval & International Compliance
The present study was conducted under the ethical principles of the Declaration of Helsinki. All participants provided informed consent before participation. The study was approved by the ethics committee of the School of Medicine and Pharmacy of Rabat under the number (No.14/19), before its launch. Participants signed an informed consent form after receiving detailed information about the study's objectives, procedures, and potential risks. Participant data was anonymized to ensure confidentiality. Additionally, the study complied with local regulations regarding human subject research.
2.5. Statistical Analysis
The statistical analysis was performed using SPSS (version 13.0). The mean (SD) or numbers and percentages described patient characteristics. Costs were presented by the mean ±SD, median, and range with minimum and maximum. Kolmogorov-Smirnov test demonstrated that the distributions of direct costs were skewed. Hence, we used a series of non-parametric univariate analyses. Mann–Whitney U-tests and Kruskal–Wallis H-tests to identify the effects of the dichotomous and polychotomous variables respectively, on direct costs. P < 0.05 were considered statistically significant.
3. RESULTS
3.1. Sociodemographic and Clinical Data of the Study Population
One hundred and ten patients with RA provided data of one year follow-up for the present survey. The mean age of the study population was 50.5 years old and ranged between 19 and 73 years old, with more than 85% of women. Further, 44.5% were married and about 55% had children. Around 47% of the participants were illiterate and 32.7% had a primary school level, while 47.3% declared that they were homemakers and 34.5% left work because of the illness. Besides, the average monthly household income was less than $250 for most (82%) and 73.6% of the patients had the RAMED Table 1.
| - | N (%) | Mean ± SD | Median (range) | Min – Max |
|---|---|---|---|---|
| Age | - | 50.53 ± 13.86 | 52 (41 ;63) | 19 – 73 |
| BMI | - | 22.04 ± 4.47 | 21 [19 , 25] | 14 – 37 |
|
Gender: Female Male |
94 (85.5) 16 (14.5) |
- | - | - |
|
Educational level Illiterate Primary Secondary University |
52 (47.3) 36 (32.7) 17 (15.5) 5 (4.5) |
- | - | - |
|
Marital status Single Married Divorced Widower |
39 (35.5) 49 (44.5) 19 (17.3) 3 (2.7) |
- | - | - |
|
Number of children 0 1-3 ≥4 |
49 (44.5) 31 (28.2) 30 (27.3) |
- | - | - |
|
Working status: Students Working Sick leave/Retired Homemaker |
11 [10] 9 (8.2) 38 (34.5) 52 (47.3) |
- | - | - |
|
Montly household income: < $250 $250 – 500 > $500 |
90 (81.8) 8 (7.3) 12 (10.9) |
- | - | - |
|
Kind of medical insurance: Ramed CNOPS CNSS Private insurance |
81 (73.6) 22 [20] 5 (4.5) 2 (1.8) |
- | - | - |
|
Early symptoms*(years) < 5 5 – < 10 10 – < 15 ≥ 15 |
12 (10.9) 22 [20] 37 (33.6) 35 (31.8) |
- | - | - |
|
Disease duration*(years): < 5 5 – < 10 ≥ 10 |
26 (27.3) 31 (28.2) 49 (44.5) |
10.14±7.03 | 9 (5,14) | 1-33 |
|
Rheumatoid factor Positive Negative |
97 (88.2) 13 (11.8) |
- | ||
|
DMARD Yes No |
76 (69.1) 34 (30.9) |
- | - | |
|
NSAID and analgesic drugs use** Yes No |
43 (39.0) 64 (58.2) |
- | - | |
|
BDMARD: Anti-CD 20 TNFα Blockers Interleukins receptors inhibitors |
64(58.2) 20(18.2) 26 (23.6) |
- | - | |
|
Surgery: Yes No |
11 (10) 99 (90) |
- | - | |
|
Comorbidity† Yes No |
53(48.2) 57(51.8%) |
- | - | |
As regards clinical background, the early symptoms and the disease duration were at least 10 years for 65% and 44.5% of patients respectively.
All the patients were under biological therapy “BDMARDs”. Anti-CD 20 (Rituximab) was the most commonly used by 58.2% of patients, while 23.6% and 18.2% used interleukin receptors inhibitors (Tocilizumab) and received tumor necrosis factors (TNF blockers) (Golimumab, Adalimumab, Infliximab, and Etanercept) respectively. In addition, for 69.1% of patients, it was associated with the conventional treatment DMARDs “disease-modifying antirheumatic drugs”; and 39% took NSAIDs and antalgic drugs too.
Most of the patients (97 of 110) had positive rheumatoid factor and 48.2% reported comorbidities, including, osteoporosis (n= 32), diabetes (n=18), and fibromyalgia (n=5), as well, 11 patients underwent surgeries due to the disease (Table 1).
3.2. Total Direct Costs
The results of the ECORAM study show that the average yearly total direct costs of RA is $7,659 per patient, with a minimum and a maximum of $1,889.5 and $29,158.3 respectively; 98% belong to the medical charges. Besides, the total direct costs of the first semester were higher than the second semester ($4,561.2 vs $3,097.81) and almost for all healthcare categories.
The largest proportion belongs to BDMADs (67%) with an annual cost of $4,944.73, followed by hospitalization (12%) with $889. The remaining 20% include costs of surgery (5%), laboratory analysis (5%), medications (3%), DMARDs (3%), radiology (2%), doctors’ visits (1%), and transportation (2%) (Table 2).
From a societal perspective, the total direct costs of patients, health insurance organizations (CNOPS, CNSS, private insurance), and the RAMED are very different (Table 3). The RAMED paid around 47% of the total medical costs, which is $3,445.56 and the health insurance organizations (CNOPS, CNSS, private insurance) paid $2,876.7 (39%), while patients paid $1,048.65 (14%) on medical and non-medical costs.
| - | Mean ± SD | S1 | Mean ± SD | S2 | Mean ± SD | Annual |
|---|---|---|---|---|---|---|
|
Median (25 ;75) |
Median (25 ;75) |
Median (25 ;75) |
||||
| Physician visits | 50.61 ± 39.58 | 36.0 (24.0 ; 64.87) |
56.47 ± 71.16 | 42 (12.0 ; 70.5) |
85.68±94.56 | 48 (26.2 ; 110.12) |
| Hospitalization | 666.86 ±474.76 | 576 (391 ; 843) |
207.74 ± 305.17 | 108 (0.00 ; 275) |
888.99 ±657.11 | 788 (503.75 ; 1,129) |
| Radiology | 107.01 ± 80.03 | 101.6 (53; 148.9) |
35.73 ± 71.06 | 0.00 (0.00 ; 22.5) |
167.26 ±150.65 | 123.7 (76 ; 208.2) |
| Laboratory analysis | 278±189.83 | 213.4 (144.78 ; 369.71) |
132.29 ± 182.43 | 73.8 (55.57 ; 115) |
334.38 ±257.8 | 284.4 (190.87 ; 387.72) |
| DMARD | 103.34 ±83.24 | 127.4 (0.00 ; 139) |
91.9 ± 97.56 | 85 (0.00 ; 113) |
195.26±137.4 | 222 (85 ; 254.57) |
| BDMARD | 2,797.85 ±3,325.19 | 1160 (580 ; 4,310.1) |
2,370.18 ± 2,719.39 | 973.5 (0.00 ; 4,321) |
4,944.73 ±5,211.25 | 1,834.1 (1,160 ; 8,364.9) |
| Medications | 154.72 ±150.69 | 118.1 (53.5 ; 162.8) |
100.39 ± 165.64 | 56.3 (14.77 ; 137.15) |
253.6 ±226.8. | 174.4 (111.9 ; 310.32) |
| Surgery | 307.27 ±1368.96 |
0.00 (0.00 ; .00) |
40.9 ± 245.43 | 0.00 (0.00 ; 0.00) |
341.63±1371.20 | 0.00 (0.00 ; 0.00) |
| Medical equipment | 5.36 ±18.53 | 0.00 (0.00 ; .00) |
0 ± 1 | 0.00 (0.00 ; 0.00) |
5.45 ±18.53 | 0.00 (0.00 ; 0.00) |
| Physiotherapy | 9.6 ±35.736 | 0.00 (0.00 ; .00) |
0.5± 4.77 | 0.00 (0.00 ; 0.00) |
10.05 ±35.93 | 0.00 (0.00 ; 0.00) |
| Transportation | 80.56±90.03 | 49.5 (24 ; 95.2) |
61.63 ± 92.31 | 30 (12 ; 60) |
142.194 ±152.4 | 98 (38.55 ; 200.5) |
| Total | 4,561.21± 3,804.38 |
3,129 (2,226.6 ; 5,807.1) |
3,097.81± 2,881.27 |
1,834.1 (774.25 ; 5,263.9) |
7,659.04 ± 5,893.12 |
4,992.5 (2,969.37 ; 11,124.35) |
| - | - | S1 | S2 | Annual | |||
|---|---|---|---|---|---|---|---|
| Mean ± SD |
Median (25 ;75) |
Mean ± SD |
Median (25 ;75) |
Mean ± SD |
Median (25 ;75) |
||
| Patient | 758.04± 1,369.73 | 434.050 (242.3 ; 701.72) |
290.59 ±331.85 | 222.6 (119.7 ; 305.2) |
1,048.65 ±1410 | 664.35 (477.5 ; 963.7) |
|
| RAMED* | 2,012.31± 2,099.74 |
1,688.15 (0.00 ; 2,258.4) |
1,433.25 ±2,208.52 | 487.7 (0.00 ; 1,880) |
3,445.56 ±4,010.79 | 2,251.7 (0.00 ; 3,729.47) |
|
| Health insurance organizations** | 1,567.28±3729.954 | 0.00 (0.00 ; 1,854.1) |
1,309.42±2,677.36 | 0.00 (0.00 ; 660.67) |
2,876.70 ±5,837.96 | 0.00 (0.00 ; 3,776.55) |
|
| Total | 4,561.21± 3,804.38 |
3,129 (2,226.6 ; 5,807.1) |
3,097.81 ±2,881.27 | 1,834.1 (774.25 ; 5,263.9) |
7,659.04± 5,893.12 | 4,992.5 (2,969.37 ; 11,124.35) |
|
3.3. Factors Associated with Total Direct Costs
Sociodemographic factors were significantly associated with total direct costs of RA: marital status (p=0.018), number of children (p=0.009), working status (p=0.005), monthly household income (p=0.001), and kind of medical insurance (p=0.000).
Additionally, several clinical factors related to RA seem to affect significantly the total direct costs as well as disease duration (p=0.023), to undergo surgery (p=0.007), DMARDs intake (p=0.029), NSAIDs and antalgic drugs intake (p=0.018) and the class of BDMARDs receiving (p=0.000) (Tables 4 and 5).
4. DISCUSSION
To our knowledge, this study is the first in Morocco to report all medical direct costs collected exhaustively from patients and related files.
ECORAM study estimated direct costs per year in patients with RA in Morocco and demonstrates that the mean total yearly direct costs in RA are about $7,659 per patient, with a minimum and a maximum of $1,889.5 and $29,158.3. The first semester's direct costs were higher than the second semester's costs ($4,561.2 vs $3,097.81). Medical costs represent 98% of the total direct costs, whilst BDMARDs costs were by far the dominating RA-related direct cost with 67% of total costs and hospitalization with 12%, and the rest of 20% consist of costs of surgery, laboratory analysis, medications, DMARDs, radiology, doctors’ visits, and transportation.
Even in the American continent, the USA ($3,173), Canada ($2575), and Argentina ($2083.9) [19-21]. However, we could not compare those findings with our results since the patients in those studies were not all under biological therapy.
Indeed, a recent Moroccan study estimated the annual costs of biological therapies in RA patients (n=197) and found a median of $1,807.57 for each patient, with an annual direct cost varying between $1,598.2 and $10,725.97. Also, reported that the overall cost of biological agents (during the 1-year follow-up) is very high ($1,062385.38) and contrasts with the Moroccan interprofessional guaranteed minimum wage of $265 per month [11]. In the present study, the overall cost of biological agents for 110 patients for one year is $543,920.48, which is under the finding of Fellous et al. proportionally to the sample size.
Researchers from France reported from an over 4-years follow-up study that the main predictors of higher costs were biologic agents use, especially, first-year biologics users, which incurred the highest levels of total costs. The mean annual direct total costs per treatment strategy group were $3,921.67 for all patients and $1,083.56, $2,086.78, $16,188.3, $9,203.77 respectively for no DMARDs, synthetic DMARDs only, first year of biologic treatment and later year of biologic treatment users [22], which is much higher than our finding.
The survey of Klimes et al. from the Czech Republic found a mean annual direct costs similar to our finding of $7821.63, among patients with and without biological treatment [23]. However, patients with biological therapy had 6.44 times higher direct costs than patients without it ($13,759.52 vs $ 2448.33) which is similar to the French study finding and very high compared with the direct costs found in this study.
According to, a Chinese study the total direct costs were $3,444. Though, about half of the medical costs ($1,721) were related to drug costs, of which biological agent represented the largest part (48.2%) with $829, although only 10.0% of the cohort had received the biological therapy [24].
In a study conducted in Turkey in 2016, the average annual cost per RA patient was $5,378.73, less than our finding ($7,659). The reason may be that only 35.4% of patients were under biological agents, which decreased the medical costs [6].
Our results confirmed that the economic burden incurred by RA is very high for the study population since the majority are poor, vulnerable, and have a monthly household income of less than $250. Besides, more than 80% were women with low educational levels and were homemakers or left work because of the illness. Moreover, 73.6% of them had the RAMED (ministry of health), which supports almost all the medical costs.
| - | N (%) | Mean ± SD | Median (range) | Min – Max | p* |
|---|---|---|---|---|---|
|
Age (years) ≤ 50 > 50 |
53 (48.2) 57 (51.8) |
7,535.40 ± 5,075.79 7,773.99 ± 6,606.51 |
5,066.1 (2,998.8 ; 11,091.4) 4,311.5 (2,745.5 ; 11,763.6) |
2,515.7 -18,984 1,889.5 – 29,158.3 |
0 .611 |
|
Gender: Male Female |
16 (14.5) 94 (85.5) |
8,088.18 ± 5,489.1 7,585.99 ± 5,983.89 |
6,763.3 (2,562.57 ; 13,032.72) 48,741.50 (2,983.92 ; 11,071) |
2,389.4 – 16,710.9 1,889.5 – 29,158.3 |
0.786 |
|
Marital status Single Married Divorced Widower |
39 (35.5) 49 (44.5) 19 (17.3) 3 (2.7) |
8,553.67 ± 4,437.80 6,213.47 ± 4,984.78 10,321.33 ± 9,140.92 2,778.43 ± 552.58 |
8,683.3 (4,755.8 ; 12,456.2) 3,534.3 (2,892.4 ; 10,580.95) 4,992.5 (3,416.5 ; 1,898.4) 2,459.4 (2,459.4 ; -) |
2,515.7 – 16,710.9 1,889.5 – 17,058.3 2,212.1 – 29,158.3 2,459.4 – 3,416.5 |
0.018 |
|
BMI: < 18,5 18,5 – 24,9 25 – 29,9 ≥ 30 |
25 (22.7) 50 (45.5) 27 (24.5) 8 (7.3) |
6,225.38 ± 5,085.74 8,161.28 ± 4,982.72 6,707.35 ± 5,354.72 12,212.12 ±11,639.53 |
3,241.4 (2,838.1 ; 10,504.75) 6,872.8 (3,175.17 ; 12,842.4) 4,992.5 (2,542 ; 11,071) 4,236.2 (3,580.8 ; 25,519.05) |
2,212.1 – 18,984 2,410.4 – 16,710.9 1,889.5 – 18,605.5 3,416.5 – 29,158.3 |
0.126 |
|
Number of children: 0 1-3 ≥4 |
49 (44.5) 31 (28.2) 30 (27.3) |
8,642.52 ± 5,116.3 6,033.52 ± 7,233.69 7,732.37 ± 5,348.91 |
8,683.3 (3,416.5 ; 12,649.3) 3,241.4 (2,729.1 ; 4,992.5) 5,979.5 (3,003.65 ; 12,155.17) |
2,459.4 – 18,984 2,212.1 – 29,158.3 1,889.5 – 16,542.6 |
0.009 |
|
Working status: Students Working Sick leave Homemaker |
11 [10] 9 (8.2) 38 (34.5) 52 (47.3) |
11,552 ± 4,704.88 5,940.83 ± 3,034.86 5,373.03 ± 3,798.28 8,803.45 ± 6,996.7 |
12,842.4 (10,898.4 ; 15,910.9) 4,160.9 (3,278.1 ; 8,683.3) 3,475.4 (2,658.6 ; 7,692.72) 5,472.85 (3,008.5 ; 15,426.45) |
2,910.2 – 16,710.9 2,515.7 – 10,111.1 1,889.5 – 14,388.9 2,212.1 – 29,158.3 |
0.005 |
|
Monthly household income: < $250 $250 – 500 >$500 |
90 (81.8) 8 (7.3) 12 (10.9) |
6,896.86 ± 5,744.62 8,523.03 ± 5,997.78 12,799.32 ± 4,484.77 |
4,100.7 (2,885.3 ; 9,824) 7,679.05 (3,241.4 ; 13,032.72) 13,490.95 (11,055.85 ; 16,542.6) |
1,889.5 – 29,158.3 2,766 – 18,605.5 3,227.7 – 17,058.3 |
0.001 |
|
Kind of medical insurance: Ramed CNOPS CNSS Private insurance |
81(73.6) 22 (20) 5 (5.5) 2 (1.8) |
5,867.92 ± 4,484.77 13,530.28 ± 6,843.43 72,881.60 ± 2,010. 16,542.6 ± 0.000 |
3,416.5 (2,727.05 ; 9,824) 15,420.2 (6,706.62; 16,442.62) 8,683.3 (5,195.45 ; 8,683.3) 16,542.6 (16,542.6 ; 16,542.6) |
1,889.5 – 18,984 4,073.7 – 29,158.3 4,311.5 – 8,683.3 16,542.6 –16,542.6 |
0.000 |
| - | N (%) | Mean ± SD | Median (Range) | Min-max | p* |
|---|---|---|---|---|---|
|
Early symptoms: < 5 5 < – < 10 10 < - < 15 > 15 |
12 (10.9) 22 (20) 37 (33.6) 35 (31.8) |
7,552.93 ± 5,632.24 5,637.12 ± 3,738 8,459.12 ± 6,960.96 8,161.30 ± 6,023.81 |
4,755.8 (2,916.62 ; 13,542.45) 3,745.1 (2,864.92 ; 10,346) 6,982.3 (2,944.3 ; 10,898.4) 4,311.5 (2,899.5 ; 15,407.7) |
2,389.4 – 16,710.9 2,212.1 – 1,357.9 1,889.5 – 29,158.3 2,459.4 – 18,984 |
0.597 |
|
Disease duration: < 5 5 < - < 10 ≥ 10 |
26 (27.3) 31 (28.2) 49 (44.5) |
5,178.32 ± 4,276.59 7,184.87 ± 5,666.35 9,230.97 ± 6,513.46 |
3,728.5 (2,682.32 ; 4,992.5) 3,241.4 (2,885.3 ; 11,071) 8,683.3 (3,415.8 ; 13,876.3) |
2,389.4 – 16,710.9 2,212.1 – 18,984 1,889.5 – 29,158.3 |
0.023 |
|
Rheumatoid factor: Positive Negative |
97 (88.2) 13 (11.8) |
8,070.04± 6,070.08 4,592.34 ± 30,212 |
5,879.64 (2,949.65 ; 11,924.3) 3,416.5 (2,868.8 ; 4,992.5) |
2,212.1 – 29,158.3 1,889.5 – 13,579.5 |
0.12 |
|
Surgery Yes No |
11 (10) 99 (90) |
12,267.25 ±78,085.48 7,147± 5,455.98 |
12,456.2(6,079.4 ; 14,388.9) 4,073.7 (2,899.5 ; 11,050.8) |
5,066.1 – 29,158.3 1,889.5 – 2,645.8 |
0.007 |
|
DMARDS No Yes |
34 (30.9) 76 (69.1) |
10,617.56 ±7,772.19 6,335.48 ± 4,260.33 |
11,476.75 (2,938.65 ; 15,710.2) 42,362 (2,929.92 ; 9,824) |
2,389.4 – 29,158.3 1,889.5 – 18,605.5 |
0.029 |
|
NSAID and analgesic drugs No Yes |
64(58.2) 43(39.1) |
6,369.65 ± 5,281.28 8,744.06 ± 5,305.63 |
3,759.7 (2,795.8; 10,701.57) 8,683.3 (3,348.4 ; 13,363.7) |
1,889.5 – 26,458.3 2,212.1 – 18,605.5 |
0.018 |
|
BDMARD Anti-CD 20 TNFα blockers Interleukins receptors inhibitors |
64 (58.2) 20 (18.2) 26 (23.6) |
3,760.04±1,985.37 13,117.48± 7,126.35 13,057.75±3,134.18 |
3,147.55 (2,667.57 ; 4,006.15) 10,898.4 (7,112.72 ; 18,889.37) 13,876.3(10,815.87 ;15,552.25) |
1,889.5-12,456.2 4,311.5-29,158.3 4,755.8-17,058.3 |
0.000 |
|
Comorbidity Yes No |
53(48.2) 57(51.8) |
7,243.37 ± 6,562.32 8,045.53 ± 5,224.32 |
4,040.5 (2,725.0 ; 11,071) 6,763.3 (3,215.25 ;12,117.4) |
2,212.1 – 29,158.3 1,889.5 – 18,984 |
0.104 |
For patients with a monthly household income of less than $250 which represents about 82% of our population, the annual average direct costs of RA was $6,896.86. The patients paid $1,048.65 and the rest was supported for the majority by the RAMED or a few of them by health insurance organizations. However, the costs paid by the patient, which include medical costs and non-medical costs (transportation) are about 35% of the annual household income of those patients.
In contrast, RAMED supported the main proportion of medical costs with 47% ($3,445.56) followed by insurance health organizations (CNOPS, CNSS, private insurance) with 39% ($2876).
In France, the total direct medical costs were from the public payer perspective and societal perspective $10,006.13, and $12,764.98 respectively [25]. From the payer’s perspective, if we consider the RAMED as the public payer and the insurance health organization and the patients as the societal, the annual total direct costs are respectively $3,445.56 and $3,925.35, which is very low in comparison with the results of the French survey.
Indeed, (Fig. 1) depicts that the GDP per capita [26] in most countries is considerably higher than the direct costs of RA treatment, both with and without biotherapy, except in Morocco. These disparities in direct costs and GDP highlight the complex interplay of healthcare systems, treatment accessibility, and economic resources in managing RA.
The comparison of direct costs of Rheumatoid Arthritis with biotherapy in Morocco, the Czech Republic, and France reveals intriguing insights. Morocco's direct costs of RA with Biotherapy are significantly higher at $7,659 compared to those in the other two countries.
In contrast, the Czech Republic and France, with higher GDPs per capita of $23,665 and $40,495 respectively, demonstrate higher economic affluence. Their direct costs of RA with Biotherapy are $13,759 and $16,188 respectively.
Despite Morocco's higher direct costs of RA with Biotherapy, the total direct costs, including the population with Biotherapy, remain lower than those of the Czech Republic and France. This suggests that the overall burden of RA management in Morocco may be lower compared to the other two countries.
Further investigations are needed to understand the factors affecting these differences and to develop adequate interventions to reduce the direct costs of RA treatments in Morocco. Policymakers can use the comparison of direct costs and GDP data to address the economic challenges of managing RA and ensure access to effective treatments worldwide.
Statistical analysis indicated that for the following subgroups of patients, the total direct costs were higher: divorced and single; without children; student and homemaker; with monthly income >$500 and with private insurance. The hypothesis could be that divorced, single, and childless patients expend more money on medical expenses since they have no additional charges for children. Students as they are still young, and because the disease is progressive and to avoid the deterioration of their health, parents do not skimp on the medical charges of their kids. Concerning patients with monthly income >$500 and private insurance, they can spend more on medical costs than patients with less income.
Furthermore, patients with a disease duration of 10 years and more; patients not taking DMARDs, patients taking NSAIDs and antalgic drugs, patients who underwent surgeries, and patients receiving the biological therapy interleukins receptors antagonists and TNF antagonists, had higher yearly direct costs.
The Czech study found that age, biological treatment, and disease duration were significant predictors of overall costs [23]. The Chinese study reported too that the disease duration is predictor of total costs. Besides, the longer the duration of the disease, the less effective the treatment, the more likely the destruction of joints and impairment of workability, and consequently the higher the cost of illness [24], which is under two other German studies [27, 28].
As concerns DMARDs, the additional charges paid by the patients not taking it could be explained by the fact that most of them used TNF blockers or interleukin receptor inhibitors for the biological therapy, which are more expensive than anti-CD 20 [29].
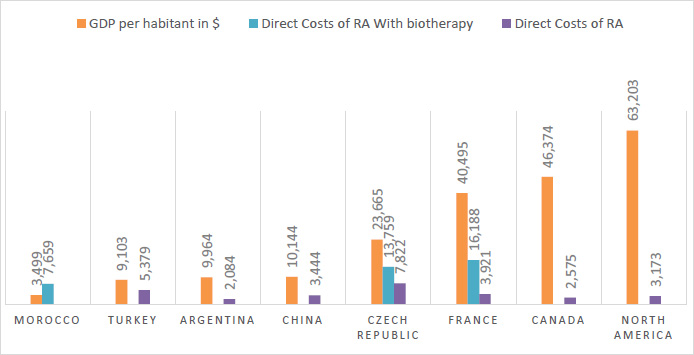
GPD per capita in $ and direct costs of RA in several countries.
This finding may contribute to comprehending the economic impact of RA in Morocco and assessing the costs associated with RA and the expenses related to various biotherapies that could be considered when determining appropriate treatment options for the disease. In addition, decision-making committees, include professors and practitioners who rely on such surveys and evidence-based statistics to build a system based on real-life results to effectively support a therapeutic strategy and to better manage the distribution of health resources.
Our study presents some limitations. Firstly, the study was not multicenter. it was exclusively conducted in a public hospital, without including the private sector, which might introduce bias. However, it's important to note that EL AYACHI hospital serves as the national reference center for rheumatology, catering to patients from all provinces of the country. Secondly, we did not include patients on DMARDs alone. This exclusion could have allowed for a comparison of medical costs and an assessment of factors affecting patients without BDMARDs. Thirdly, the study was conducted among patients treated in a public hospital, which explains the low income of the population. While this factor may act as a confounder, it does not impact the consumed resources, population follow-up, or the overall cost of the pathology. It is worth mentioning that the management of rheumatoid arthritis (RA) remains consistent, whether in a public or private hospital. The divergence lies mainly in reimbursement methods. In private hospitals, patients often have insurance coverage or pay out of pocket, while in public hospitals, most patients are covered under RAMED.
Nonetheless, our study considered various parameters of RA patients and highlighted the association of several sociodemographic and clinical factors with the total direct costs of RA in Morocco.
Indeed, our findings are likely to be generalizable nationwide, as well as to some neighboring countries. This is due to the therapeutic approach adopted in our population, which aligns with recommendations from the “Société Marocaine de Rhumatologie (SMR)”, adapted from the European Alliance of Associations for Rheumatology (EULAR) recommendations. This alignment reinforces the potential generalizability of these results.
CONCLUSION
In conclusion, this study presents a global overview of the total direct costs of RA among patients with biological therapy in Morocco, which were estimated to be $7,659 per patient per year, with a minimum and a maximum of $1,889.5 and $29,158.3. In addition, 98% belongs to medical costs.
The biological agent’s treatment was the dominating direct cost with 67% of total costs ($4,944.73), hospitalization 12% ($889), and the remaining 20% consist of the other medical and non-medical costs ($1,825).
RAMED supported the main proportion of direct costs with $3,445.56 followed by insurance health organizations (CNOPS, CNSS, private insurance) with $2,876.7, while patients paid $1,048.65 (14%) on medical and non-medical costs.
For the most part of the published studies and the present study too, biological agents’ costs are the most significant contributor to the total direct costs. However, in order to conduct a global evaluation, it is crucial to estimate the indirect costs of RA. On the other hand, the quality of life is the ultimate object to assess the impact of therapeutic innovation on chronic and expensive diseases.
This finding may contribute to a better understanding of the economic impact of RA in Morocco and also, would provide useful data for governmental decision-makers in the distribution of health resources.
AUTHORS' CONTRIBUTION
The authors confirm their contribution to the paper as follows: study conception and design: H.Z., S.H., H.R., F.A., R.B.; analysis and interpretation of results: H.Z., A.C.H., M.S. L.L.; planning: H.R., F.A., R.B., S.A. ; overall direction: S.A. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| RA | = Rheumatoid arthritis |
| BMC | = Basic Medical Coverage |
| CHI | = Compulsory Health Insurance |
| RAMED | = Medical Assistance Program |
| CNSS | = National Social Security Fund |
| CNOPS | = National Fund of Social Security Organizations |
| NRP | = National Reference Pricing |
| RBSMR Registry | = The Moroccan Registry of biological therapies in rheumatic diseases |
| ACR | = American College of Rheumatology |
| HIS | = Hospital Informatics System |
| BDMARD | = Biological Disease-Modifying Antirheumatic Drugs |
| DMARD | = Disease-Modifying Antirheumatic Drugs |
| NSAID | = Non-steroidal Anti-inflammatory Drug |
| USD | = United States Dollar |
| GDP | = Gross Domestic Product |
| SMR | = Société Marocaine de Rhumatologie |
| EULAR | = European Alliance of Associations for Rheumatology |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The Ethical Committee of the School of Medicine and Pharmacy of Rabat, Morocco approved this study before its initiation (Approval No. 14/19).
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were under the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
A clear and detailed informed consent form was explained to all patients and signed prior to their inclusion in the study.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of this article are available at [El Ayachi Hospital in Salé in hard copy format and within the non-public Hospital Information System (HIS)] for patient-related data. Regarding price-related information, it is publicly accessible via the following links: https://anam.ma/anam/regulation/tarification-nationale-de-reference/ and www.medicament.ma] for drug pricing.
ACKNOWLEDGEMENTS
Declared none.


